Overview
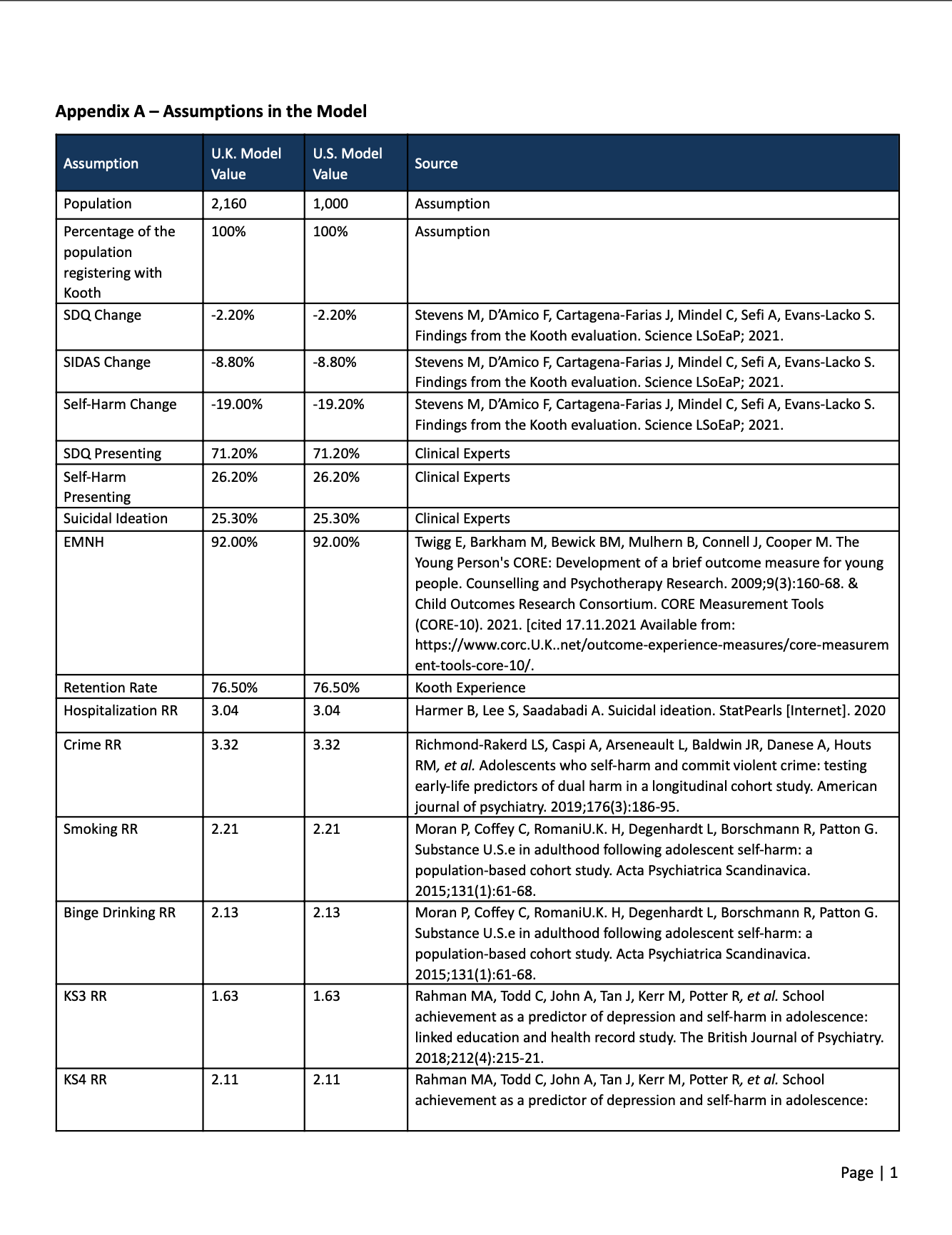
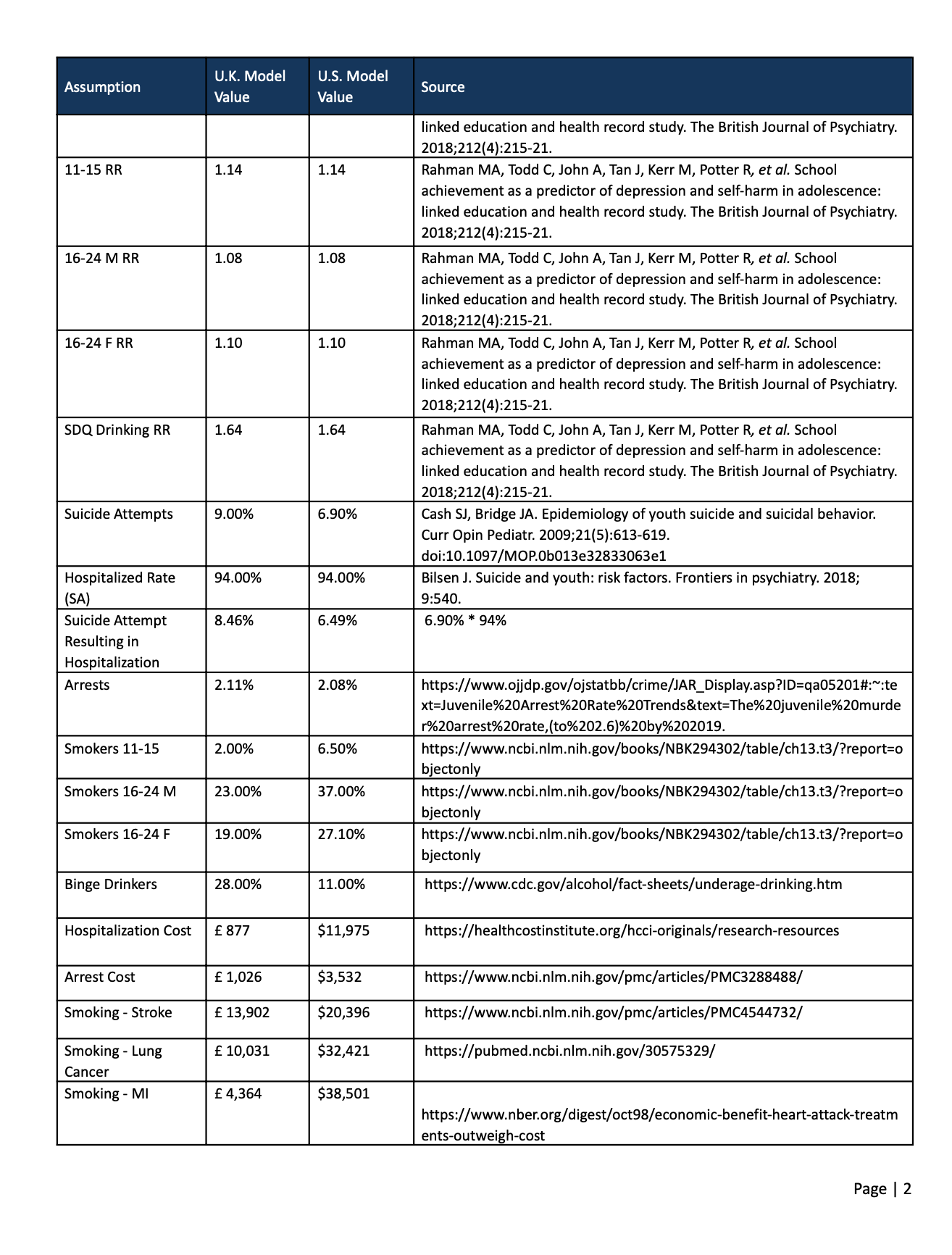
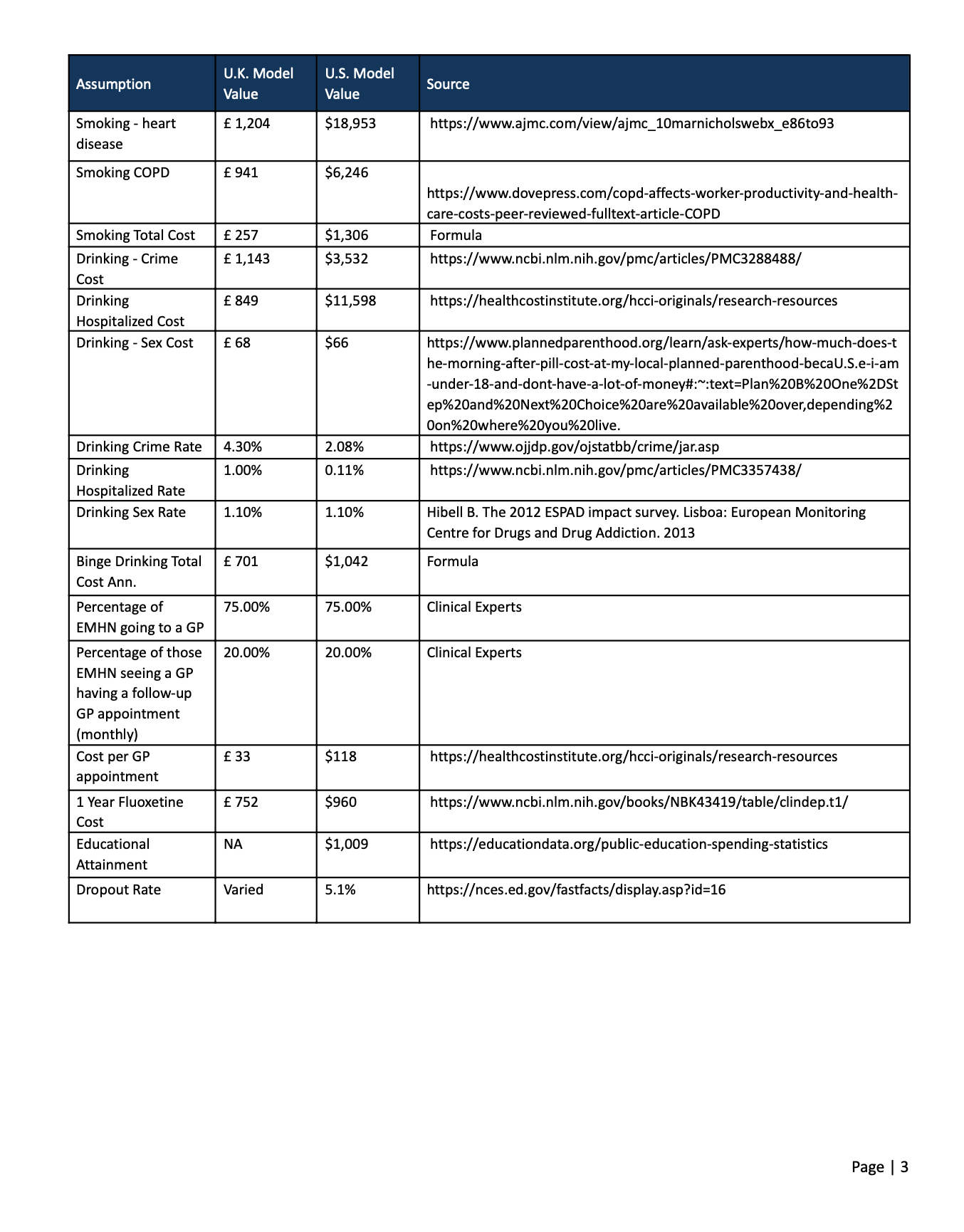
Mental health among American youth has reached a crisis. With limited existing resources, many children and young people lack the ability to seek appropriate treatment. A scalable and easily accessible service could provide a solution to this public health emergency. The Kooth platform is a mental health web-based platform that is proven to successfully manage the mental health needs of children and young people (CYP) at scale. This work aims to convert a United Kingdom (U.K.)-based evaluation and estimate the potential benefits of the Kooth program in the United States (U.S.) marketplace, including medical cost savings and reduction in negative mental health outcomes.